Featured
Table of Contents
Note: The complying with criteria use to grownups, teenagers, and children older than 6 years. For kids 6 years and younger, see the DSM-5 area titled "Posttraumatic Stress Disorder for Kid 6 Years (even more ...) Michael is a 62-year-old Vietnam expert. He is a separated dad of 2 youngsters and has four grandchildren.
He describes his childhood as separated. His dad physically and mentally abused him (e.g., he was beaten with a switch up until he had welts on his legs, back, and butts). By age 10, his moms and dads regarded him as incorrigible and sent him to a reformatory school for 6 months. By age 15, he was making use of cannabis, hallucinogens, and alcohol and was often truant from school.
How to Look For about an experienced EMDR Practitioner for EMDR intensives

In one event, the soldier he was following to in a bunker was fired. Michael really felt helpless as he spoke to this soldier, that was still mindful. In Vietnam, Michael enhanced his use both alcohol and cannabis. On his return to the USA, Michael continued to consume and use cannabis.
His life supported in his early 30s, as he had a steady task, encouraging close friends, and a relatively stable family life. However, he divorced in his late 30s. Shortly thereafter, he wed a 2nd time, yet that marital relationship ended in separation as well. He was chronically distressed and depressed and had sleep problems and regular nightmares.
Success Statistics for EMDR and ART Therapy
In the 1980s, Michael got numerous years of mental health and wellness therapy for dysthymia. In the mid-1990s, he returned to outpatient treatment for comparable signs and symptoms and was identified with PTSD and dysthymia.
He reported that he really did not like how alcohol or other substances made him feel anymorehe really felt out of control with his feelings when he utilized them. Michael reported signs and symptoms of hyperarousal, invasion (intrusive memories, nightmares, and preoccupying thoughts concerning Vietnam), and avoidance (separating himself from others and feeling "numb"). He reported that these signs seemed to connect to his childhood misuse and his experiences in Vietnam.
Pairing Eye Movement Desensitization and Reprocessing together with Adjunctive Therapeutic Methods
For instance, seeing a flick concerning child abuse can set off signs and symptoms associated with the trauma. Various other triggers include going back to the scene of the injury, being reminded of it in a few other way, or noting the anniversary of an event. Likewise, battle professionals and survivors of community-wide catastrophes may appear to be coping well soon after a trauma, just to have signs and symptoms arise later when their life situations appear to have actually supported.
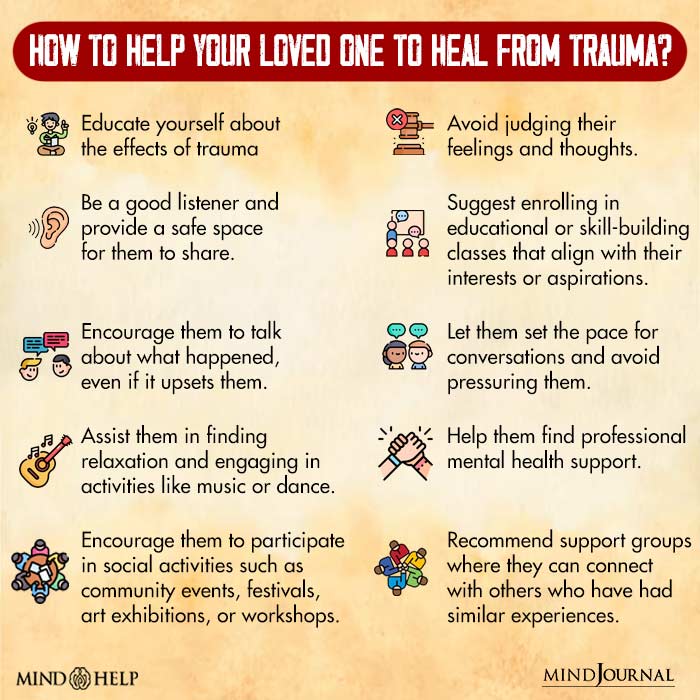
Attract a connection in between the injury and presenting trauma-related symptoms. Produce a risk-free environment. Discover their assistance systems and fortify them as required. Understand that triggers can precede stressful anxiety responses, consisting of postponed reactions to trauma. Recognize their triggers. Create coping techniques to navigate and take care of symptoms. Although study is restricted throughout societies, PTSD has actually been observed in Southeast Asian, South American, Center Eastern, and Native American survivors (Osterman & de Jong, 2007; Wilson & Tang, 2007).
Body Symptoms in Eye Movement Desensitization and Reprocessing Therapy in Calgary, AB
It would be perceived as inappropriate and perhaps bastardizing to focus on the emotional distress that she or he still bears. (For a review of cultural competence in treating injury, describe Brown, 2008.)Approaches for determining PTSD are also culturally particular. As component of a project started in 1972, the World Health And Wellness Company (THAT) and the National Institutes of Health And Wellness (NIH) embarked on a joint research study to examine the cross-cultural applicability of classification systems for different medical diagnoses.
Hence, it prevails for trauma survivors to be underdiagnosed or misdiagnosed. If they have not been recognized as trauma survivors, their psychological distress is often not connected with previous trauma, and/or they are detected with a problem that marginally matches their presenting symptoms and emotional sequelae of trauma. The complying with areas offer a short overview of some psychological conditions that can arise from (or be gotten worse by) terrible stress.
The term "co-occurring conditions" describes instances when a person has several mental illness along with several material usage disorders (consisting of substance misuse). Co-occurring problems are common among people who have a background of injury and are seeking assistance. Just people particularly educated and certified in psychological health and wellness assessment must make diagnoses; trauma can result in difficult situations, and several signs can be existing, whether they satisfy complete analysis requirements for a certain disorder.
Much more research is now analyzing the several possible pathways amongst PTSD and other conditions and just how different sequences influence medical discussion. There is clearly a connection between trauma (consisting of individual, team, or mass trauma) and material make use of as well as the presence of posttraumatic tension (and various other trauma-related conditions) and material utilize conditions.
Addressing Chronic Anxiety via EMDR
Likewise, individuals with substance use problems go to higher risk of establishing PTSD than individuals that do not abuse materials. Counselors collaborating with trauma survivors or customers who have compound usage disorders have to be especially familiar with the possibility of the various other problem developing. People with PTSD typically contend the very least one added diagnosis of a mental illness.
There is a threat of misunderstanding trauma-related signs in compound abuse treatment settings. For instance, evasion signs in a private with PTSD can be misinterpreted as lack of motivation or unwillingness to take part in compound abuse therapy; a counselor's initiatives to attend to substance abuserelated habits in very early healing can likewise provoke an overstated reaction from a trauma survivor who has profound terrible experiences of being trapped and regulated.
PTSD and Compound Use Disorders: Essential Treatment Realities. PTSD is one of the most typical co-occurring psychological conditions located in clients basically misuse treatment (CSAT, 2005c). People in therapy for PTSD often tend to abuse a wide variety of substances, (more ...) Maria is a 31-year-old female detected with PTSD and alcoholism.
Table of Contents
Latest Posts
Treating Social Anxiety through Eye Movement Desensitization and Reprocessing for Trauma therapy
Starting Your Therapeutic Journey with Eye Movement Therapy for Accelerated Resolution Therapy
Assisting Each Other Within Private Healing with Play Therapy
More
Latest Posts
Treating Social Anxiety through Eye Movement Desensitization and Reprocessing for Trauma therapy
Starting Your Therapeutic Journey with Eye Movement Therapy for Accelerated Resolution Therapy
Assisting Each Other Within Private Healing with Play Therapy